How to make make an informed choice of breast screening modality
To screen or not to screen? If yes, which technology suits you? These questions are critical for women concerned about the statistics on breast cancer. Breast cancer is second only to lung cancer as a leading cause of cancer death in women (1). The earlier breast cancer is diagnosed, the better the chances that the woman will have a more favorable outcome. According to the Center for Disease Control (CDC) statistics, the mortality rates for breast cancer have been declining steadily by 1.9% per year from 2003 through 2012 (1). This decline is a direct reflection of early detection through screening and advances in treatment. So, it is important for the woman to be well informed about the different modalities available for breast screening.
Clinical Breast Examination
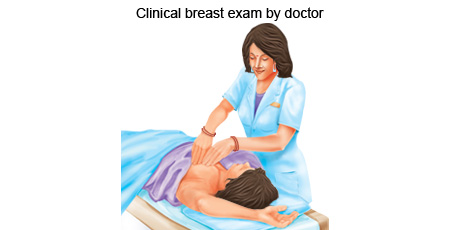
CBE has been a part of the annual preventive well-woman examination for decades. CBE must be performed by a trained clinician, who checks for breast appearance i.e. size and shape, skin covering the breast for any rash, dimpling, or other abnormal signs, nipples for any discharge, lumps by palpation.
Mammography
Mammography is a gold standard for screening and diagnostic tool for breast cancer. Mammography captures the picture of the breast using X-rays. The basic objectives of mammography are to identify densities, micro-calcifications, and asymmetry. The main shortcoming of conventional mammography is a decrease in sensitivity with the overall sensitivity measured at approximately 70% (2). The standard 2-view digital mammogram does not detect all cancers with the sensitivity decreasing as the density of breast tissue increases. In women with dense breast tissue, almost 76% of cancers are missed (2). Mammography is relatively expensive (3), women are exposed to radiation, and an expert is required to interpret the scan image.
Digital Breast Tomosynthesis (film screen mammography)
This is a digital clinical imaging procedure where an X-ray tube rotates across an arc and takes pictures at different angles of the breast resulting in a 3D image (4). Mammography combined with DBT requires a dose of radiation approximately double than used for mammography alone (4). The advantages of DBT are becoming apparent with its improved sensitivity for cancer detection and improved specificity resulting in less false positives. However, it requires a trained radiologist, is expensive and there is considerable exposure to radiation (3).
MRI (Magnetic Resonance Imaging)
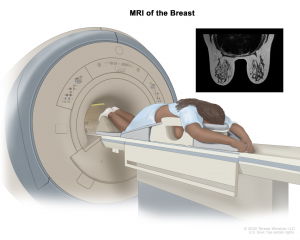
MRI measures changes in the movement of protons in fat and water with the application of changing magnetic fields, which is different across the tissues (5). It acquires an image by processing the signal changes that occur following application of pulses of energy. Advantages of MRI include the very high true positive rates and the sensitivity of MRI imaging (5). However, MRI is very expensive, approximately 10 times more than the cost of a standard screening mammogram (3) and the invasive nature of the procedure because the patient must be injected with intravenous gadolinium (5).
Breast Ultrasonography
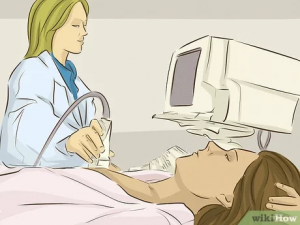
Ultrasonography can detect smaller cancer lesions in women with dense breasts in comparison with standard digital mammography (6). Additionally, it is relatively inexpensive, readily available, and requires no injected contrast or ionizing radiation (3). However, it needs qualified personnel for interpretation, there can be lack of uniformity in assessing the scans. In conclusion, the time needed to do the scan as well as the skill necessary to detect small, non-palpable tumors using hand-held ultrasound limits its universal implementation.
Gaps in current screening methods:
- Non-affordability
- Difficult accessibility
- Possibility of radiation or dye exposure
- Pain
- No appropriate tests for women <45 years
- Sensitivity is affected by density of Breasts
Thermalytix
Thermalytix is a machine learning and artificial intelligence-based solution developed by NIRAMAI that uses the thermogram (heat map) of a person’s body to detect early signs of cancer (7).
The system consists of a thermal camera that captures thermal images of the breast, a computer that processes the images, and software that interprets the results as shown in figure 1, for the scan, the patient is asked to stand about 3 feet in front of the camera with her arms raised over her head while views of the breast are taken as shown in figure 2.


Advantages of Thermalytix
- Affordable
- Portable, light, small screening device
- No radiation
- It can detect cancer long before lump is felt
- Non-contact, non-invasive, privacy aware
- Can detect cancerous tumors with 91% sensitivity and 82% specificity (8)
Thermalytix has also been able to identify malignant tumors in women who had no clinical signs of cancer. Further, results from the published clinical trials for Thermalytix show that machine learning can be used to provide a safe, privacy-aware, affordable, and automated solution for the detection of early-stage breast cancer. In conclusion, the high sensitivity of Thermalytix shows its potential for use as frontline screening modality for breast cancer.
References:
- Key, Timothy J., Pia K. Verkasalo, and Emily Banks. “Epidemiology of breast cancer.” The lancet oncology 2.3 (2001): 133-140.
- Holland R, Mravunac M, Hendriks JH, Bekker BV. So-called interval cancers of the breast. Pathologic and radiologic analysis of sixty-four cases. Cancer. 1982 Jun 15;49(12):2527-33. doi: 10.1002/1097-0142(19820615)49:12<2527::aid-cncr2820491220>3.0.co;2-e. PMID: 7074569
- Feig, Stephen. “Cost-effectiveness of mammography, MRI, and ultrasonography for breast cancer screening.” Radiologic Clinics 48.5 (2010): 879-891.
- Chong, Alice, et al. “Digital breast tomosynthesis: concepts and clinical practice.” Radiology 292.1 (2019): 1.
- Morrow, Monica, Janet Waters, and Elizabeth Morris. “MRI for breast cancer screening, diagnosis, and treatment.” The Lancet 378.9805 (2011): 1804-1811.
- Hooley, Regina J., Leslie M. Scoutt, and Liane E. Philpotts. “Breast ultrasonography: state of the art.” Radiology 268.3 (2013): 642-659.
- Sudhakar, S., et al. “Thermalytix: an advanced artificial intelligence based solution for non-contact breast screening.” International Journal of Medical and Health Sciences 12.2 (2018): 48-51.
- Singh, Akshita, et al. “Multicentric study to evaluate the effectiveness of Thermalytix as compared with standard screening modalities in subjects who show possible symptoms of suspected breast cancer.” BMJ open 11.10 (2021): e052098.

